introduction
Borderline Personality Disorder (BPD) is a serious mental health condition that affects how people think, feel, and behave. It can lead to unstable relationships, extreme emotions, and difficulty managing stress. In this blog post, we’ll explore what BPD is, its common signs, its causes, and practical strategies for managing the condition effectively.
What is Borderline Personality Disorder (BPD)?
Borderline Personality Disorder is a mental health disorder that primarily affects a person’s emotional regulation and self-identity. Those with BPD may experience rapid shifts in their mood, frequent feelings of emptiness, and an intense fear of abandonment. These emotional challenges can interfere with their day-to-day lives and relationships.

Symptoms of Borderline Personality Disorder (BPD)
Borderline Personality Disorder (BPD) is a mental health condition that affects how a person thinks, feels, and interacts with others. The symptoms of BPD can be severe and challenging, often causing instability in relationships and emotions. In this article, we will explore the common symptoms of Borderline Personality Disorder, helping you understand what to look for if you suspect someone may be living with this condition.
1. Intense Mood Swings
One of the hallmark symptoms of Borderline Personality Disorder is extreme mood swings. People with BPD may experience rapid shifts in their emotional state, often without a clear reason. They might go from feeling happy or excited to feeling deeply sad or angry in a very short time. These mood swings can be triggered by everyday events, making it hard to predict how a person with BPD might react to a situation.

2. Fear of Abandonment
Individuals with BPD often experience an overwhelming fear of being abandoned or rejected, even in situations where there is no real threat. This fear can lead to behaviours such as clinging to others, becoming overly dependent, or, conversely, pushing people away in an attempt to prevent perceived abandonment. This fear may cause significant stress in personal relationships.

3. Unstable Relationships
People with Borderline Personality Disorder often have intense, unstable relationships. They may quickly idealise someone, seeing them as perfect, but then suddenly devalue them when they feel disappointed or betrayed. This shift in perception can cause frequent conflicts and confusion in relationships, making it difficult for people with BPD to maintain healthy, stable connections.

4. Impulsive and Risky Behavior
Impulsivity is a common symptom of BPD. Individuals may engage in reckless behaviours, such as substance abuse, unsafe sex, or reckless driving. These actions are often attempts to cope with intense emotions or to feel more in control, but they can have harmful consequences.

5. Chronic Feelings of Emptiness
Many individuals with BPD report feeling empty or hollow inside, as though something important is missing. This feeling of emptiness can be distressing and difficult to overcome, leading some to seek out external sources of validation or to engage in unhealthy coping mechanisms.

6. Intense Anger or Difficulty Controlling Anger
People with BPD can experience intense anger, often disproportionate to the situation. This anger can be difficult to control and may lead to outbursts, arguments, or violent behavior. The inability to manage these intense feelings of anger can create challenges in both personal and professional life.

7. Self-Harm or Suicidal Behavior
One of the more severe symptoms of Borderline Personality Disorder is self-harm, such as cutting or burning. Some individuals with BPD may also experience suicidal thoughts or attempt suicide, often as a way to cope with emotional pain or feelings of worthlessness.

8. Distorted Self-Image
People with BPD may struggle with an unstable sense of self, causing them to feel confused about who they are. Their self-image may shift dramatically from one moment to the next, and they may feel like they have no clear identity or purpose. This lack of self-definition can lead to challenges in making decisions or setting life goals.

9. Paranoia or Dissociation
In times of stress, people with Borderline Personality Disorder may experience symptoms like paranoia or dissociation. They may feel disconnected from reality or believe that others are out to harm them. This can lead to feelings of mistrust or detachment, making it difficult to interact with others.

Conclusion
The symptoms of Borderline Personality Disorder can be overwhelming and affect many aspects of a person’s life. Intense emotional fluctuations, unstable relationships, and impulsivity are common features of the disorder. However, with the right treatment and support, individuals with BPD can manage their symptoms and lead fulfilling lives. If you or someone you know is struggling with BPD, seeking professional help is the first step towards recovery.
What Causes Borderline Personality Disorder (BPD)?
Understanding the causes of Borderline Personality Disorder (BPD) is essential for both diagnosis and treatment. While the exact cause remains unclear, experts believe that BPD develops as a result of a combination of genetic, environmental, and brain-related factors. In this article, we’ll explore the various factors that contribute to the development of BPD.
1. Genetic Factors
Genetics plays an important role in the development of Borderline Personality Disorder. Research suggests that BPD tends to run in families, indicating a hereditary component. People who have a close family member, such as a parent or sibling, with BPD are more likely to develop the disorder themselves. However, while genetic factors increase the risk, they alone do not guarantee that someone will develop BPD.

2. Childhood Trauma and Abuse
One of the most significant environmental factors in the development of BPD is early childhood trauma. Many individuals with BPD have experienced physical, sexual, or emotional abuse during their formative years. These traumatic experiences can cause lasting emotional damage, leading to difficulties in regulating emotions and maintaining stable relationships.
Abandonment, neglect, or growing up in an unstable or unpredictable environment can also contribute to the development of BPD. These experiences can create deep fears of rejection or abandonment, which are common symptoms of the disorder.

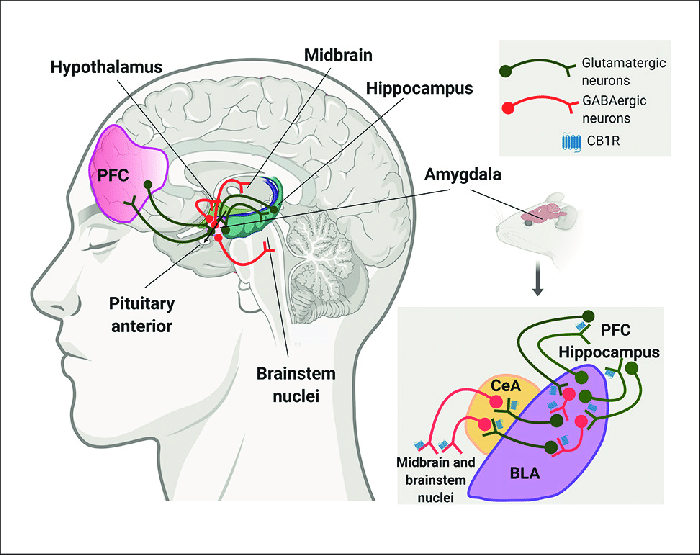
3. Brain Structure and Function
Studies have shown that certain areas of the brain may function differently in individuals with Borderline Personality Disorder. For example, research suggests that the amygdala, which is involved in emotional regulation, may be overactive in people with BPD. This could lead to heightened emotional responses to situations. Additionally, the prefrontal cortex, which helps regulate emotions and behaviour, may not function as effectively, making it harder to control impulses or manage intense feelings.
These brain differences are believed to play a role in the emotional instability and impulsivity often seen in people with BPD.
4. Abnormalities in Social and Cognitive Development
Some researchers believe that Borderline Personality Disorder can develop when an individual’s social and cognitive development is impaired. Children who grow up in environments where they don’t receive proper emotional support or care may struggle to develop healthy coping mechanisms. Without these tools, they may resort to destructive behaviours or difficulty managing emotions as they get older.
This lack of proper emotional development can lead to difficulties in relationships, trouble with self-esteem, and a distorted sense of identity — all of which are common in BPD.

5. Environmental Factors
In addition to childhood trauma, other environmental factors can influence the development of Borderline Personality Disorder. Stressful life events, such as the loss of a loved one, bullying, or relationship breakdowns, can trigger or worsen symptoms in people who are already predisposed to BPD. Growing up in an environment with inconsistent or chaotic behaviour from caregivers can also contribute to emotional instability.
These environmental stressors may interact with genetic factors, making it more likely for someone to develop BPD.
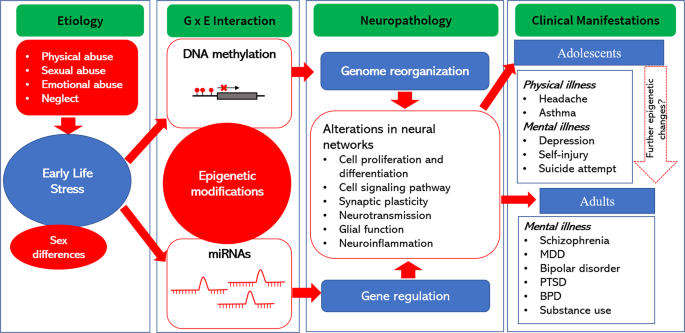
6. Interaction of Multiple Factors
Most experts agree that Borderline Personality Disorder is not caused by just one factor but by an interaction of multiple elements. Genetics may provide a predisposition to the disorder, but it’s the combination of childhood trauma, brain differences, and environmental stressors that ultimately lead to the development of BPD. The disorder often develops over time as a result of these combined influences.

Conclusion
The causes of Borderline Personality Disorder are complex and multifaceted. Genetic predispositions, childhood trauma, brain abnormalities, and environmental stressors all contribute to the development of BPD. While these factors can increase the likelihood of developing the disorder, they do not guarantee it. Understanding the causes of BPD is key to providing appropriate treatment and support for those affected.
How to Manage Borderline Personality Disorder (BPD) Effectively?
Managing Borderline Personality Disorder (BPD) can be challenging, but with the right strategies, support, and treatment, individuals can lead fulfilling lives. BPD often causes emotional instability, difficulty with relationships, and impulsivity, but these symptoms can be managed effectively with the right approach. In this article, we’ll explore practical ways to manage BPD and improve overall well-being.
1. Seek Professional Help
The first step in managing Borderline Personality Disorder is to seek professional help. A qualified therapist, especially one trained in Dialectical Behaviour Therapy (DBT), can be invaluable in teaching coping skills and emotional regulation strategies. DBT is a form of cognitive behavioural therapy (CBT) specifically designed for people with BPD. It focuses on helping individuals manage emotions, reduce self-destructive behaviours, and improve relationships.
Psychiatrists may also recommend medications to help manage symptoms like depression, anxiety, or mood swings, although there is no medication specifically for BPD.

2. Practice Emotional Regulation
One of the key challenges of BPD is emotional instability, but it’s possible to manage this with regular practice. Learning how to identify and regulate emotions is essential in reducing impulsivity and preventing mood swings. DBT includes strategies such as mindfulness, distress tolerance, and emotion regulation skills that can help individuals with BPD understand and control their emotions more effectively.

3. Build Strong Support Networks
Having a solid support system is crucial in managing Borderline Personality Disorder. Support from family, friends, or support groups can provide encouragement and understanding. It’s important to be open about your condition with trusted individuals so they can offer support when needed. Support groups for BPD can also be beneficial, as they provide a safe space to share experiences and learn from others who understand the challenges of the disorder.

4. Develop Healthy Coping Mechanisms
People with BPD often use unhealthy coping mechanisms, such as self-harm or substance abuse, to manage overwhelming emotions. Learning and adopting healthier ways to cope with stress and emotional pain is essential. Some effective coping strategies include:
Mindfulness: Practicing mindfulness helps individuals stay grounded in the present moment, reducing the emotional intensity of distressing thoughts and feelings.
Physical Activity: Regular exercise can improve mood, reduce stress, and promote overall well-being.
Creative Outlets: Activities like journaling, painting, or music can serve as outlets for emotional expression.

5. Establish Healthy Routines
Having a consistent daily routine can provide structure and stability, which are important for managing Borderline Personality Disorder. Regular sleep patterns, balanced meals, and physical activity contribute to better mental health. Setting small, achievable goals each day can also provide a sense of accomplishment and reduce feelings of chaos or emptiness.

6. Set Boundaries in Relationships
Individuals with BPD often struggle with unstable relationships, which can be worsened by intense emotional reactions or fear of abandonment. Learning how to set and maintain healthy boundaries is crucial for improving relationships. Communicating openly with friends, family, and romantic partners about needs, feelings, and expectations can help avoid misunderstandings and conflicts.

7. Be Patient with Yourself
Managing Borderline Personality Disorder takes time, and it’s important to be patient with yourself during the process. Progress may be slow, and setbacks are common, but with the right treatment and support, improvement is possible. Celebrate small victories, and remember that self-compassion is key to recovery.

Conclusion
Managing Borderline Personality Disorder (BPD) effectively involves a combination of professional help, emotional regulation skills, a strong support network, and healthy coping strategies. While BPD can be challenging, it is possible to manage the symptoms and live a fulfilling life with the right tools and support. If you or someone you know is struggling with BPD, reaching out for professional help is an important first step.
Change and Hope for the Future in Borderline Personality Disorder (BPD)
Living with Borderline Personality Disorder (BPD) can feel overwhelming, but it’s important to remember that change is possible, and there is hope for the future. While managing BPD may seem challenging at times, with the right treatment, support, and strategies, individuals can make significant progress and lead fulfilling lives. In this article, we’ll discuss the potential for change in BPD and the hopeful outlook for those living with the disorder.
1. The Possibility of Recovery
One of the most important things to remember when managing Borderline Personality Disorder is that recovery is possible. Although BPD is a complex condition, many individuals experience improvements over time with proper treatment and support. Therapy, such as Dialectical Behaviour Therapy (DBT), has been shown to be highly effective in helping individuals with BPD manage their symptoms and improve their quality of life. While BPD is not something that is “cured,” people can learn to manage their symptoms and achieve stability.
2. The Role of Therapy in Change
herapy is a key factor in creating positive change for people with Borderline Personality Disorder. Dialectical Behaviour Therapy (DBT), in particular, focuses on teaching emotional regulation, mindfulness, and coping skills. Through DBT, individuals can gain better control over their emotions and behaviours, reduce impulsivity, and improve their relationships. Over time, these skills help individuals feel more in control of their lives, leading to greater stability and well-being.
Other therapeutic options, such as Cognitive Behavioural Therapy (CBT), can also help address negative thought patterns and behaviours that contribute to the symptoms of BPD. Therapy can provide the tools needed to build a healthier, more positive future.

3. Building Healthy Relationships
Another area of hope for individuals with Borderline Personality Disorder is the ability to build and maintain healthy relationships. One of the key symptoms of BPD is difficulty in relationships, but through therapy and personal growth, individuals can learn how to set boundaries, communicate more effectively, and understand their emotional needs. By developing healthier coping mechanisms and emotional regulation skills, people with BPD can improve their interactions with others and build lasting, supportive relationships.

4. The Importance of Support Systems
Having a strong support system is essential for managing Borderline Personality Disorder. Family, friends, and support groups can provide encouragement, understanding, and a sense of belonging. A support system can help individuals with BPD feel less isolated and more connected to others, fostering emotional healing and stability.
Support groups, in particular, provide a space for individuals to connect with others who understand the challenges of living with BPD. Sharing experiences and learning from others who have faced similar struggles can provide hope and motivate individuals to continue working toward change.

5. Medication as a Tool for Managing Symptoms
While there is no medication specifically for Borderline Personality Disorder, medication can be helpful in managing certain symptoms, such as depression, anxiety, or mood swings. Antidepressants, mood stabilisers, or antipsychotic medications may be prescribed to help individuals manage their emotional experiences and reduce the severity of certain symptoms. Medication, when used in conjunction with therapy, can significantly improve the quality of life for people with BPD.

6. The Power of Self-Compassion
Another key element in finding hope for the future is practising self-compassion. Individuals with Borderline Personality Disorder often experience intense self-criticism, which can contribute to feelings of hopelessness. Learning to be kind and patient with oneself is essential for recovery. Acknowledging that progress takes time and celebrating small victories along the way can provide the motivation needed to continue moving forward.

7. A Bright Future
With the right tools and mindset, there is hope for the future for those living with Borderline Personality Disorder. The journey may be challenging, but positive change is always possible. By seeking therapy, building support systems, and practising self-care, individuals with BPD can create a brighter, more stable future for themselves. Recovery is not a straight path, but each step forward brings new opportunities for healing and growth.

Conclusion
There is always hope for change, even for those living with Borderline Personality Disorder. With the right treatment, therapy, support systems, and personal effort, individuals with BPD can experience significant improvements in their emotional well-being and relationships. By focusing on recovery and growth, individuals with BPD can create a future filled with stability, happiness, and a sense of peace.
Conclusion: Borderline Personality Disorder (BPD)
In conclusion, Borderline Personality Disorder (BPD) is a complex condition that affects many aspects of a person’s life, including emotions, relationships, and behaviour. However, with the right treatment, support, and strategies, individuals with BPD can manage their symptoms and lead fulfilling lives. While the path to recovery may be challenging, it is possible to achieve emotional stability and improve relationships through therapies like Dialectical Behavior Therapy (DBT), support from family and friends, and the development of healthy coping mechanisms.
It’s important to remember that Borderline Personality Disorder is not a life sentence. Change and improvement are possible, and individuals living with BPD can make progress at their own pace. By understanding the symptoms, causes, and management strategies, people with BPD can take proactive steps towards a brighter future, filled with hope and stability.
With professional guidance, emotional regulation, and a strong support network, those with BPD can create lasting change and enjoy a better quality of life. If you or someone you know is struggling with BPD, seeking help from a healthcare professional is the first step towards managing the condition effectively.